Cardiovascular disease (CVD) and Diabetes care disparities among African Americans and Intervention to reduce disparities
Final Project for courses:
- Health Communication in the Information Age (LSC 617)
- Communication Arts, Race and Health Communication (COM ARTS 612)
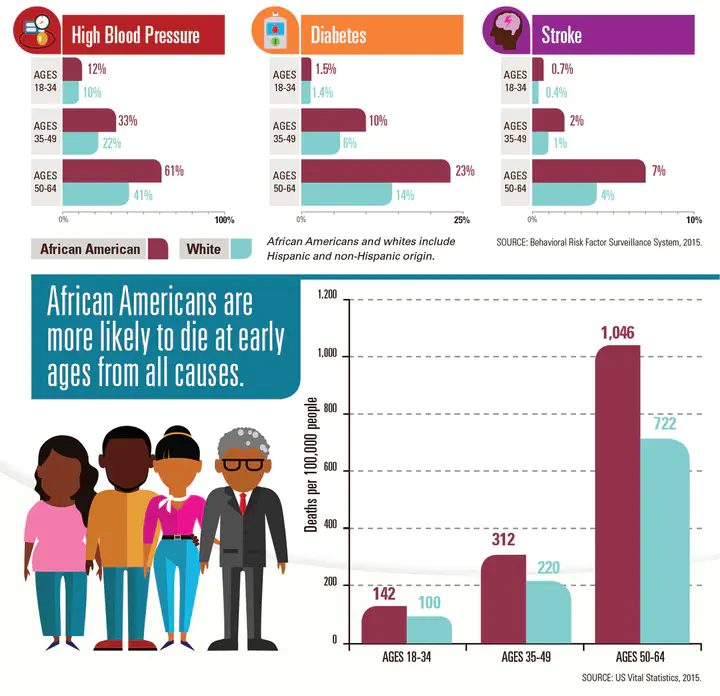
Adults with diabetes are more likely to report a history of cardiovascular disease (CVD) than those without diabetes. African Americans have the highest incidence of diabetes, heart disease, and stroke, tend to be younger at the time of first stroke event, and their strokes tend to be more severe with higher morbidity and result in higher mortality. The causes of health disparities are complex and include societal issues such as institutional racism, discrimination, socioeconomic status, poor access to health care lack of health insurance, poor understanding of the relationship between obesity, diabetes, and CVD among low-income African American communities. In addition, community-level barriers, such as limited access to supermarkets with healthy food items, can lead to unhealthy dietary habits. However, the prevalence of these chronic diseases across racial groups cannot be solely explained by socioeconomic status. Regardless of the ability to speak and understand English, speaking a language other than English at home confers a higher risk for not receiving appropriate health care. Therefore, changes at the policy level for equal access to high-quality care are paramount to reducing health care disparities. Higher morbidity and mortality rates caused by CVD and diabetes can lead to higher care costs in patients and a disproportionate burden on African Americans.

Higher morbidity and mortality rates caused by cardiovascular disease (CVD) and diabetes can lead to higher care costs in patients, and a disproportionate burden is on minorities. Therefore, addressing the causes of these disparities and utilizing intervention to control CVD and diabetes in one of the largest minority groups in the US, i.e., African Americans, can potentially decrease healthcare costs.
The goal of this study was to assess the causes of diabetes and CVD health disparities among African populations and investigate what intervention are out there to mitigate disparities. These disparities other than SES include patient provider relationship (implicit biases), medical mistrust and community level barriers. Centuries of racial discrimination led to medical mistrust among African Americans and lingering effects persists decades after Tuskegee Syphilis Study.
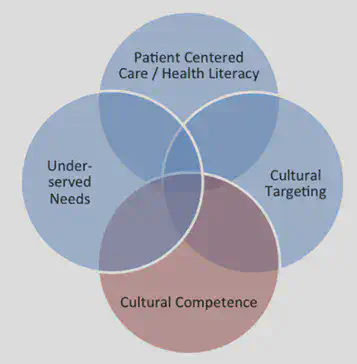
We explored interventions to mitigate these disparities. Those interventions include improving access to care and quality of care. Interventions to eliminate the Black-White disparity in CVD and diabetes control would avert thousands of deaths from CVD in Black Americans. These CVD and diabetes disparities indicate underlying variations in health behavior, medical treatments and need to evaluate causes of these difference and targeted intervention efforts. The health care disparities trends have implications for policy makers, public health practitioners and clinicians to move towards cardiovascular health equity for African Americans. Addressing the causes of these disparities and proposing intervention can decrease health care costs and burden for African Americans.
References
Baumgartner, J., Collins, S., Radley, D., & Hayes, S. (2020). How the Affordable Care Act (ACA) Has Narrowed Racial and Ethnic Disparities in Insurance Coverage and Access to Health Care, 2013‐18. Health Services Research. https://doi.org/10.1111/1475-6773.13406
Carnethon, M. R., Pu, J., Howard, G., Albert, M. A., Anderson, C. A. M., Bertoni, A. G., Mujahid, M. S., Palaniappan, L., Taylor, H. A., Willis, M., & Yancy, C. W. (2017). Cardiovascular Health in African Americans: A Scientific Statement From the American Heart Association. In Circulation. https://doi.org/10.1161/CIR.0000000000000534
Cefalu, W. T., Dawes, D. E., Gavlak, G., Goldman, D., Herman, W. H., van Nuys, K., Powers, A. C., Taylor, S. I., & Yatvin, A. L. (2018). Insulin access and affordability working group: Conclusions and recommendations. Diabetes Care, 41(6). https://doi.org/10.2337/dci18-0019